Elimination of Filariasis statement or statesmanship?
Elimination of Filariasis statement or statesmanship? the story behind it.
Elimination of Filariasis was mentioned as one of the goals within reach and a date of 2018 set for it the Feb 1st Budget speech by our Finance Minister. ,the buildup to it is far longer.
As per WHO estimates in 2000 AD, 120 million people in tropical and subtropical areas of the world cases suffered from Lymphatic Filariasis (LF) and 40 million suffered secondary problems like hydrocoel and lymphoedema (Also known as Elephentiasis or Hathi pao). As one of the leading causes of global disability, LF accounts for at least 2.8 million Disease Affected Life Years (DALYs).
India has 18 million sufferers and LF is considered endemic in East UP, Bihar, the entire coastal region as well as a few other areas. In many of these endemic regions, the legs -instead of the face are examined before confirming suitability for marriage. Similarly, a hydrocoel maybe, but not always, hidden. But it does interfere in consummating marriage, Still, disability is largely considered to be mild (20%), not high enough for even a subsidized railway ticket! Thus another, but unquoted ill effect, is depression and mental illness.
India has both main types of the worm – Wuchereria bancrofti found almost all endemic regions. It causes both hydrocoel and Lymphoedema. Brugia malayi is found only in Kerala and causes only Lymphoedema. The female worm lays live young worms (called microfilaria). These are tiny and slender enough to travel into the stomach of the mosquito along with its blood meal. After a short growth cycle, they get deposited in the skin during the subsequent blood meal of the mosquito. The microfilaria penetrates the skin and grows to an adult worm after reaching the lymphatic system.
The Filaria worm stays and feeds on lymph – a less well known component of body’s circulatory system and described in part II. To make itself comfortable, the worm dilates the lymphatic channels besides paralyzing the lymphatic hearts. This results in only a minor swelling which may reverse with death of the worm. But often, other processes called Adeno Dermato Lymphangitis Attacks (ADLA) or Filarial fever set the stage for long term affects. ADLA is generally due to bacterial infection, but can also occur due to release of microfilaria and sometimes ascribed to the dying worm itself – and is known to occur after consuming DEC.
As a consequence, lymph accumulation occurs in the dependent parts of the body, e.g. the legs or arms ( Lymphoedema) and in the scrotum (Hydrocoel). Less common affects include lymphoedema of the genital organs, passage of lymph in urine (Chyluria) and accumulation in the abdomen (Chylous ascites) or chest (Chylothorax). ADLA also kills the worm so those with secondary affects rarely can spread the disease further.
In 2000, the World Health Assembly (WHA) had set a goal of Program for Global Elimination of Lymphatic Filariasis (GPELF) by 2020. It has two components
- Elimination of the worm though Mass Drug Administration (MDA) which is somewhat similar to the Poilio eradication program. In this, Filaria killer drugs, namely DiEthyl Carbamezapine (DEC), Albendazole and Ivermectin. (The last one was the reason for the 2015 Noble prize to the inventor) are provided in various combinations to the entire population of the endemic district on a designated annual Filaria day
- Morbidity control i.e. treatment for those with effects. This is important because even though Filaria does initiate Hydrocoel and Lymphoedema, killing the worm, except in very early cases, has little affect in reversing it
Various affected countries are in different stages of GPELF and the exact combination of MDA drugs varies. China eliminated the disease long time back by salt fortification of DEC.
India uses two drugs for MDA Albendazole with DEC. After a few pilots, the formal nationwide launch was in 2005. It was expected that over 5 years, if more than 65% population – consumed the drug, the incidence of disease prevalence would decrease to < 1%, and the area can considered filaria free. The mosquitos are unable to spread it further. India had announced its successful PELF completion target year to be 2015. It was postponed to 2017 and now as per announcement in the budget speech, to 2018.
Thanks to PELF, the number of endemic districts has fallen from 250 to 138. However, the end is not so near, largely because compliance is as low as 25% in many areas. Besides, there is an understanding that Filariasis is prevalent in areas beyond the designated 250 districts. These too need targeting. To accelerate the program, Ivermectin is being added, making MDA triple drug.
State and district level filaria officers run the MDA, as well as morbidity control programs. They do the assessment regarding endemicity, arrange for availability of medicines and ensure that the same is provided to each household through personal visits by ASHAs and Health Workers. The health workers also monitor for reactions to the drugs which are minor. A few deaths occurred in Tamilnadu during the pilot phase (2003-4). These after investigation, were ascribed to contamination of DEC, so care on that side is also important.
Morbidity control has many components, ASHA workers get paid Rs 250 for identifying and reporting the patient with disease. They are offered treatment by the government, Surgery can be done for Hydrocoel and a sum of ₹750 is budgeted as compensation for the surgical team. A Lymphoedema patient is told that meticulous leg washing is the only treatment that is needed and a sum of ₹150 given to the patient for purchase of a bucket and soap! From the author’s viewpoint there are weaknesses in the Morbidity control component and contribute to poor compliance to PELF.
Leg washing and hygiene does prevent ADLA but does not stop it all together. It does little for the swelling which is a reason for mental and physical disability, Since this swelling is lymph – a good culture medium, an insect bite, minor injury or even wet feet due to a extra rainy day can trigger the attack. ADLA is also know to occur just after MDA probably as a reaction to the dying worm. Hence, many victims and their families refuse to take the drugs.
Also there are some worrying reports of understating the disease incidence. In 2015, Sangtin, a community based NGO in Sitapur District UP, contacted SATHI – a technical NGO helping Lymphoedema patients for help. Sangtin wass asked to get some figures of incidence to justify action by SATHI. An occurrence of 262 patients was reported from 13 villages. Since Sitapur, was reportedly having a total of 4117 cases ( figures with government), SATHI reported in the National Medical Journal of India that actual incidence is 10 times higher. The government wanted additional proof, so a repeat survey was done in June 2016, this time covering 183 villages or the entire Pisawan block. The results – 5% of the population is suffering which means 200000 patients in Sitapur district alone!
Treatment is possible and should be done especially for Lymphoedema – the main neglected component which we discuss in part II.
Part II – Lymphoedema and its management
, A resolution was passed in the US Senate in 2016 declaring 6th March as Lymphoedema Day, due to efforts by an organization called Lymphatic Education & Research Network ( LE&RN). The effort was to highlight the incidence of the disease as well as stop willful neglect of such patients through media events and workshops. The India chapter of LE&RN and SATHI collobrated with AIIMS New Delhi and the governments’ cell looking after Filrariais (VBDCP) to hold . This year’s event is planned at AIIMS Bhubhaneshwar for 5th and 6th March.
The human body is 90% water. 60% inside the cells, 5% in blood and the rest in between allowing constant movement of food and Oxygen from the blood to the cells and return back of waste like CO2 and urea, to the blood. Thicker waste, like proteins, dead cells, bacteria etc does not enter the blood stream directly. These go through separate channels called lymphatics, which can be rightly called the body’s sewage system. Lymphatic channels have intervening filters called Lymph Nodes to check for harmful material. Once found they activate immunity, phagocytose the proteins and otherwise, make it clean to enter the blood stream which is done after lymph travels up to the neck. These lymph nodes are found specific points like the groin or axilla and higher up. Till the fluid reached the node, the immune reaction to the bacteria is relatively ineffective.
Lymphatics are very fine channels, mostly occurring in and just under the skin. Movement of fluid for the limbs is antigravity. This is assisted by minute internal hearts (smooth muscle) and limb movements like standing walking or running. The expansion and contraction of muscles compresses the vessels against the skin and helps propel the fluid up. Blood propulsion in veins is largely similar except that these have valves and no internal hearts.
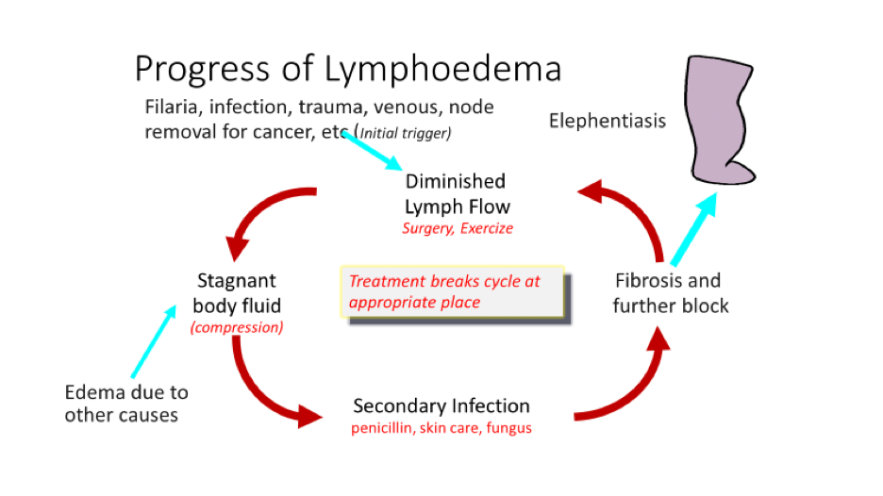
Accumulated lymph, like milk or any other body fluid, is an excellent culture medium. Bacteria entering after minor cuts, insect bites even through blood from carious teeth etc are more likely to turn into full fledged ADLA. Sores following fungal infection and which is common between the toe webs and skin folds due to sweating, also in fishermen and those working in the rice fields is a common source. ADLA triggers a vicious and relentless cycle of Blockage and destruction of Lymph channels, leading back to fluid accumulation and even more chance of infection (see diagram). There is poor reach to the lymph nodes hence immunity is less. With each attack, the swelling becomes less reversible. Maggots, fungus and other infection also leads to poor hygiene and the person becomes smelly, withdrawn and depressed.
1% of the World’s population suffers from Lymphoedema. In the US, which does not have filariasis, it affects 25 million people. Lymphoedema also occurs because of non filarial causes of which the most common is following successful treatment for cancer – notably of the breast and reproductive organs. Other causes include poor formation of lymphatic channels since birth, recurrent infections, venous disease, after limb injury, old age, paralysis or even infection supervening in edema caused by heart, kidney or liver disease. ADLA are common features of all these causes and hence the treatment is also largely similar which is to find methods to break the vicious cycle of oedema, infection and blockage.
Unfortunately knowledge that this problem is treatable is missing not only among patients but to a large extent among the medical community. Lymphoedema is a chronic disease. Though a cure is not possible, it can be managed with long term prospects no better or worse than diabetes or hypertension the other better known chronic diseases. Swelling can almost completely disappear, with cosmetic improvement, ADLA is less likely and one can lead a near normal life.
The treatment is known as CDT or Complete Decongestive Therapy – a judicious mix of compression of the limb through bandages, garments or pumps, massage along with exercise. Wrong application can make the patient worse.This is a specialized treatment, administered in western countries by specially trained nurses and physiotherapists who are simply called (Lymphedema) therapists.
In India, very few trained persons exist and it is thought that the treatment is costly. So, the only treatment the government is offering them is a bucket of water and soap! However, research at a clinic in New Delhi as well as at AIIMS has shown that the most important component of CDT is simple compression with bandages. Not only is it inexpensive, but also the technique of how to tie can be taught to the patient himself.
his was recently tested in over 100 rural agricultural workers of Sitapur District, UP. Patients were examined for the problems, told how to wash the leg and then in groups of 20 or 25 each, were provided bandage sets which they not only tied themselves but also assisted their neighbours. Monthly follow up was done with the help of voluntary field workers with monitoring through Telemedicine. The results have been remarkable. Plans are afoot to start centres across the country offering a range of care from simple rural camps to specialized surgery


